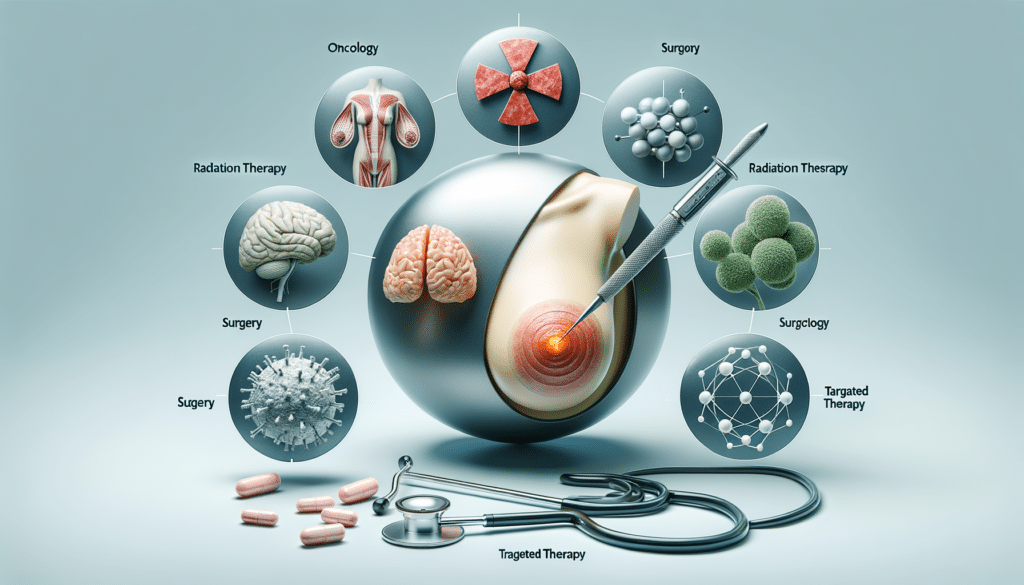
Understanding Breast Cancer Treatment
Breast cancer is a complex disease that requires a multifaceted approach to treatment. The journey from diagnosis to remission is often paved with a variety of treatment options, each tailored to the unique needs of the patient and the specific characteristics of the cancer. Understanding these options is crucial for patients and their families to make informed decisions. This section delves into the various treatment modalities available, highlighting their purposes and how they contribute to managing breast cancer.
Surgery: The Cornerstone of Treatment
Surgical intervention remains a primary treatment for breast cancer, offering a direct approach to removing cancerous tissue. There are several types of surgeries available, each with its own indications and benefits. The most common procedures include lumpectomy and mastectomy. A lumpectomy, often referred to as breast-conserving surgery, involves the removal of the tumor and a small margin of surrounding tissue. This option is generally suitable for early-stage cancers and aims to preserve as much of the breast as possible.
On the other hand, a mastectomy involves the removal of the entire breast and is recommended in cases where the cancer is more widespread. Advances in surgical techniques, such as skin-sparing and nipple-sparing mastectomies, have improved cosmetic outcomes and patient satisfaction. Reconstructive surgery is often considered post-mastectomy to restore the breast’s appearance, offering patients a sense of normalcy post-treatment.
Radiation Therapy: Targeting Cancer Cells
Radiation therapy is a critical component of breast cancer treatment, particularly following surgery. It involves the use of high-energy rays to target and destroy cancer cells that may remain in the breast or surrounding areas. This treatment is typically recommended after a lumpectomy to reduce the risk of cancer recurrence. Radiation therapy can be delivered externally through external beam radiation or internally using brachytherapy.
External beam radiation is the most common form, where a machine directs radiation at the cancer site. Brachytherapy, on the other hand, involves placing radioactive material inside the body near the cancer cells. This method allows for a higher dose of radiation in a shorter period, often resulting in fewer side effects. The choice between these methods depends on various factors, including the cancer’s stage and location, as well as the patient’s overall health.
Chemotherapy: Systemic Cancer Control
Chemotherapy is a systemic treatment that uses drugs to kill cancer cells throughout the body. It is often used in conjunction with other treatments to enhance their effectiveness. Chemotherapy can be administered before surgery, known as neoadjuvant chemotherapy, to shrink tumors and make them easier to remove. Alternatively, it may be used after surgery, termed adjuvant chemotherapy, to eliminate any remaining cancer cells and reduce the risk of recurrence.
While chemotherapy is a powerful tool in the fight against cancer, it is not without its side effects. Patients may experience fatigue, nausea, hair loss, and increased susceptibility to infections. Despite these challenges, chemotherapy remains a vital option for many breast cancer patients, offering a chance to target cancer cells that may have spread beyond the breast.
Hormone Therapy: Blocking Cancer Growth
Hormone therapy is an effective treatment for breast cancers that are hormone receptor-positive. These cancers rely on hormones like estrogen and progesterone to grow. Hormone therapy works by blocking the body’s natural hormones from reaching the cancer cells or by lowering hormone levels in the body. This treatment is often used after surgery to reduce the risk of cancer recurrence and is typically administered over several years.
Common hormone therapy medications include selective estrogen receptor modulators (SERMs) and aromatase inhibitors. SERMs, such as tamoxifen, block estrogen receptors on cancer cells, while aromatase inhibitors, like anastrozole, reduce the amount of estrogen produced in the body. Hormone therapy is generally well-tolerated, though it can cause side effects like hot flashes, joint pain, and an increased risk of osteoporosis.
Targeted Therapy: Precision Medicine in Action
Targeted therapy represents a newer, more precise approach to treating breast cancer. Unlike traditional chemotherapy, which affects all rapidly dividing cells, targeted therapy focuses on specific molecules involved in cancer growth and progression. This precision reduces damage to healthy cells and minimizes side effects. Targeted therapies are often used in combination with other treatments to improve outcomes.
One of the most well-known targeted therapies is trastuzumab, which is used to treat HER2-positive breast cancer. HER2 is a protein that promotes the growth of cancer cells, and trastuzumab works by attaching to HER2 receptors on cancer cells, preventing them from receiving growth signals. This therapy has significantly improved survival rates for patients with HER2-positive breast cancer.
Other targeted therapies include CDK4/6 inhibitors and PARP inhibitors, each designed to address specific genetic mutations or pathways involved in cancer development. As research continues to advance, targeted therapy offers hope for more effective and personalized breast cancer treatments in the future.